Photo of the day: Choosing the Right Face Mask and the difference between a respirator and face mask
10 min readFace masks and coverings have become a familiar sight over the last year as we all work together to bring the coronavirus pandemic under control. But with so many on the market, are any face masks better than others and what should you be looking for in a face mask?
In the photo of today, you will be familiar with types of face mask and 3 tips for choosing the right mask in addition you will know the difference between respirator and face mask
Tips 1:So, how will I know how each mask is rated?
Simply look for ASTM Level 1, 2, or 3 on the face mask package. However, not all face masks are ASTM-rated, so it’s important to check before you choose. It’s worth the effort to find face masks that DO carry the ASTM rating, to be sure you’re getting the proper level of protection.
Tips 2:Tell me more about how masks are tested
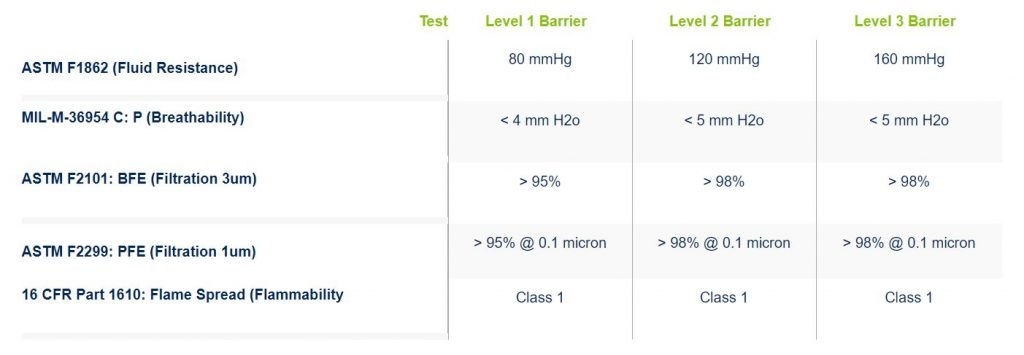
The five performance metrics and their related tests are:
- Fluid Resistance – Test ASTM F1862
This test evaluates the resistance of a medical face mask to penetration by a small volume (~2 mL) of synthetic blood at a high velocity (80 mmHg, 120 mmHg, or 160 mmHg). The mask either passes or fails based on visual evidence of synthetic blood penetration. - Breathability – Test MIL-M-36954 C: ΔP
This test determines the face mask’s resistance to airflow. A controlled flow of air is driven through the mask, and the pressure before and after is measured. The difference in pressure is divided by the surface (in cm2) of the sample. A lower breathing resistance indicates a better comfort level for the user. - Bacterial Filtration (BFE) – Test ASTM F2101
This test measures the percentage of bacteria larger than 3 microns filtered out by the mask. The challenge material used is Staphylococcus aureus. - Particulate Filtration (PFE) – Test ASTM F2299
This test measures the percentage of particles larger than 1 micron filtered out by the mask. The challenge material used consists of latex aerosol concentrations in a controlled airflow chamber. - Flammability – Test 16 CFR Part 1610: Flame Spread
This test exposes the face mask material to a flame and measures the time required for the flame to proceed up the material at a distance of 127 mm (5 inches). Class 1 means the material exhibits normal flammability and is acceptable for use in clothing.

Tips 3: Does an ASTM-rated face mask provide all the protection I need?
It protects your nose and mouth against splashes and sprays of blood and other bodily fluids, as well as bacteria and particulate matter of the sizes indicated in the above table; however, face masks do not provide respiratory protection against airborne diseases. For that purpose, a respirator is required.
What is a respirator? and what is the difference between a respirator and a face mask?
A respirator is a personal protective device that is worn on your face, covers at least your nose and mouth, requires fit-testing, and is used to reduce your risk of inhaling hazardous airborne particles (including dust particles and infectious agents), gases, or vapors.
One of the most commonly used respirators is a NIOSH-approved N95 Respirator mask, which has been tested to filter out at least 95% of airborne particles. A Surgical N95 Respirator is a NIOSH-approved N95 Respirator that has been cleared by the FDA for use as a surgical mask. Unlike other masks, N95 respirators must be fit-tested for each individual to ensure proper protection.
Is there a difference between a respirator and a surgical mask?
Yes. below we will outline some of the key differences between respirators and surgical masks. Health care workers routinely use surgical masks as part of their personal protective equipment. However, surgical masks are not respirators and are not certified as such. Non-medical masks are also discussed below.
Please also see read (breath-safely-the-proper-use-of-respiratory-protection/)
When should workers wear a respirator or a surgical mask?
The decision of whether or not workers need to use either respirators or surgical masks must be based upon a hazard analysis of the worker’s specific work environment and the protective properties of each type of personal protective equipment.
Respirators are designed to help reduce the wearer’s respiratory exposure to airborne contaminants such as particles, gases, or vapors. Respirators and filters must be selected based on the hazards present. They come in various sizes and styles and should be individually selected to fit the wearer’s face and to provide a tight seal. A proper seal between the user’s face and the respirator forces inhaled air to be pulled through the respirator’s filter material, thereby providing protection.
Surgical masks, also known as procedural or medical masks, are designed to help prevent contamination of the work environment or a sterile field from large particles generated by the wearer/worker (e.g., to prevent the spread of the wearer’s spit or mucous). Surgical masks may also be used to help reduce the risk of splashes or sprays of blood, body fluids, secretions, and excretions from reaching the wearer’s mouth and nose. Surgical masks may also be worn by patients to help limit the spread of infections.
Note that masks with an exhalation valve are not recommended because the valves allow respiratory particles to spread outside the mask (these masks do not protect others from COVID-19 nor do they help limit the spread of the virus).
Can you tell the difference between a respirator and a surgical mask just by looking at it?
The difference is not always immediately apparent. A respirator will be marked with its approval rating (e.g., N95, N100, etc.). Surgical masks do not have this rating. (Note there are also “surgical masks” that have been rated as respirators (i.e., N95 surgical masks).)
Always be sure you are wearing the right respirator or mask for the hazards present and the task you are performing.
What are some of the differences?
The table below outlines some of the key differences between respirators and surgical masks.
Note: In this blog, N95 surgical masks are included in the general category of respirators.
| Key Element | Respirators | Surgical Masks |
|---|---|---|
| Evaluation, Testing, and Certification | Respirators are evaluated, tested, and certified by National Institute for Occupational Safety and Health (NIOSH) to meet set minimum performance requirements, including filter efficiency and breathing resistance. NIOSH-approved respirators are required in Canada. A NIOSH approved respirator will have the following text printed on the respirator: NIOSH type of approval (e.g., N95), and the manufacturer’s name | The Medical Devices Bureau of the Therapeutic Products Directorate (TPD) in Health Canada is the national authority that monitors and evaluates the safety, effectiveness, and quality of diagnostic and therapeutic medical devices in Canada. Depending on the class of medical devices, certain licensing and authorization to sell in Canada are required. |
| Purpose | Respirators protect from exposure to airborne particles. In healthcare, protects from exposure to biological aerosols including viruses and bacteria. | Surgical masks are a barrier to splashes, droplets, and spit. |
| Fit (Face seal) | Respirators are designed to seal tight to the face of the wearer. Wearers should be fit tested to make sure they are using the appropriate model and size of respirator to get the best fit. | Surgical masks are not designed to seal tight against the face. |
| Filtration | Respirator filters that collect at least 95% of the challenge aerosol are given a 95 rating. Those filters that collect at least 99% receive a “99” rating. And those that collect at least 99.97% (essentially 100%) receive a “100” rating. | Surgical masks do not effectively filter small particles from the air. |
| Use Limitations | Generally, single-use. Should be discarded when it: becomes damaged or deformed, no longer forms an effective seal to the face, becomes wet or visibly dirty, breathing through it becomes more difficult, or becomes contaminated with blood, respiratory or nasal secretions, or other bodily fluids. Some types of respirators can be reused (e.g., elastomeric masks). Follow the manufacturer’s instructions. | Generally, one-time use (one patient encounter). Follow the manufacturer’s instructions. |
Source: National Institute for Occupational Safety and Health (NIOSH), 2018. Respirator Trusted-Source Information – Section 3: Ancillary Respirator Information.
What should a workplace do when respirators or surgical masks are required?
Employers should have a written respirator program that describes the procedures for selecting and using respiratory protective equipment. The correct use of a respirator is just as important as selecting the correct respirator for the hazards present.
Elements of a respirator program include:
- roles and responsibilities
- hazard assessment
- respirator selection
- training
- respirator fit testing
- use of respirators
- cleaning, inspection, maintenance, and storage of respirators
- health surveillance
- program evaluation, and
- recordkeeping
(Please see: Respiratory-protection-program/)
What should I know about non-medical masks?
Non-medical masks can reduce the volume of aerosols and microorganisms that reach others when you cough, sneeze, laugh or sing.
During a pandemic, wearing a non-medical mask may be required by your employer, provincial or territorial public health authority, or local government. The risk of contracting COVID-19 increases in situations where people are in closed spaces (with poor ventilation) and crowded places when with people from outside their immediate household. Risk is higher in settings where these factors overlap or involve activities such as close-range conversations, singing, shouting, or heavy breathing (e.g., during exertion).
In general, people may be asked to wear non-medical masks when out in public when it is not possible to maintain at least 2 meters for physical distancing, particularly in settings such as shopping areas, stores, personal service settings, public spaces (including outdoors such as markets, skating rinks, or street get-togethers), and on public transportation.
Non-medical masks can be purchased or homemade. non-medical face masks or face coverings should:
- use materials that are breathable
- be made of at least 2 layers of tightly-woven material fabric (such as cotton or linen) and a third middle layer of filter-type fabric, such as non-woven polypropylene
- be large enough to completely and comfortably cover the nose, mouth, and chin without gaps
- fit securely to the head with ties or ear loops
- maintain their shape after washing and drying
- be changed as soon as possible if damp or dirty
- be comfortable and not require frequent adjustments
Some masks also include a pocket to accommodate a filter. The filter can be a piece of non-woven polypropylene fabric (such as craft fabric, interfacing material used for sewing, or non-woven material used to make some reusable shopping bags), a paper kitchen towel that has been folded in half, or a baby wipe that has been rinsed, dried and folded in half. Reusable masks with a non-woven filter can be washed multiple times. Disposable filters should be changed daily and removed from the mask before washing.
When supplies are limited, N95 or other respirators that provide higher protection should be reserved for health care workers.
Note that some individuals may find wearing a mask uncomfortable, or experience what feels like shortness of breath, anxiety, or panic. Masks may make the air feel “stuffy”, but there is no change to the levels of oxygen or carbon dioxide a person will breathe in. If you feel you have a medical concern that limits your ability to wear a non-medical mask, discuss your concerns with your health care professional.
Masks should not be worn by anyone who is unable to remove the mask without assistance (e.g., due to their age, ability, or developmental status), including children under 2 years old. Children between 2 and 5 years old may be able to wear a mask if supervised. It will depend on their ability to tolerate it, as well as put it on and off.
When wearing a non-medical mask:
- Wash your hands before putting on the mask.
- Adjust so the mask covers your nose, mouth, and chin with no gaps.
- Do not touch the mask or your face while wearing it.
- Change the mask if it gets spoiled, such as it gets dirty or wet.
- Clean your hands before removing the mask.
- Take the mask off by using the straps. Do not touch the front of the mask.
- Wash your hands after removing the mask.
- Store masks in a paper bag, envelope, or container that does not trap moisture.
- Store clean masks separately from dirty ones.
- If you used the mask for a short time and may wear it again, store it so that the outside surface is folded towards itself (so that the outside “dirty” surfaces are touching), and place it in a paper bag or similar container.
- Do not place the mask under your chin, around your neck, off the ear, under the nose, on top of your head, or over your arm.
- Do not share a soiled reusable mask with others until it has been cleaned or laundered.
- For some people, not being able to see the other person’s face and mouth clearly may cause difficulties. Consider using a transparent (clear) mask if appropriate. Maintain at least 2 meters distance, and only the person speaking should remove their mask while communicating. Use written or digital communication where possible.
- Do not allow the mask to be a hazard to other activities, such as getting caught on equipment in the workplace or at a playground.




